I am re-publishing this article on prostate cancer developments, first posted in May 2017, in view of prostate cancer being in the news today (2/2/18). The number of men dying due to prostate cancer in the UK has been comparable with the number of women dying due to breast cancer for some years, but official figures just released show that prostate cancer deaths have now over-taken those due to breast cancer. The latest figures from 2015 show there were 11,819 deaths from prostate cancer compared with 11,442 from breast cancer. Moreover, the death rate from prostate cancer is increasing whilst that from breast cancer has been decreasing for the last 15 years.
The news articles remind us that, since 2002, more than £520m has been invested in tackling breast cancer, more than double the amount received for prostate treatment and research. That sounds like an improvement – in 2005/6 the research spend on prostate cancer was less than 30% that on breast cancer.
Nevertheless, there have been significant developments in both the diagnosis and treatment of prostate cancer. So the bigger issue may be applied health spending, rather than research spending. This was the subject of my previous post, reproduced below.
Diagnosis is the issue for prostate cancer – the prostate is not so readily accessible as a breast! In the UK it takes an average of 56 days from the time a man first reports symptoms to a GP, for him to be confirmed with prostate cancer. In 25% of cases it takes more than four months. For breast cancer, diagnosis takes on average just 14 days, largely thanks to the national screening programme of regular mammograms.
There is no national screening programme for prostate cancer. As a man you need to be pro-active in seeking a PSA test. Men over 50 are entitled to a PSA test on the NHS – although this is generally expressed with the proviso “after discussing the pros and cons with your doctor”. Many GPs or practice nurses will initially refuse you a PSA test. You may need to insist (politely). If you have symptoms and they refuse you a test, you should certainly insist. Despite the test’s shortcomings, it is the entry point for further diagnostic investigations (see the blog below).I suspect GP’s reticence may be as much financial as medical, but at £400 a go – what price peace of mind?
If you do have a PSA test, you should not have ejaculated for the previous 48 hours, nor taken part in vigorous exercise. I have had several tests – invariably organised by nurses – but never had those requirements stipulated. (I do wonder if that may be part of the problem with the test’s notorious variability).
The original post from May 2017 follows…
***************
I said I’d do a less depressing blog. Cancer may seem like a curious choice for an upbeat post, but actually there have been several pieces of good news about prostate cancer in the last few months which are worth bringing to your attention.
In the UK, around 47, 000 men are diagnosed with prostate cancer annually, and about 11,000 men die of the disease per year (roughly the same as the number of women who die from breast cancer).
There are things you can do to minimise the risk to yourself. In the UK, you need to be pro-active. The NHS will do nothing unless you make the first move.
Contents
- The PSA Test
- Prostate Biopsy
- Enhanced MRI Scans
- Targeted drug treatment via blood test
- Robotic surgery
- Transformative laser/bacteria treatment
1. The PSA Test
In the UK there is no national screening programme for prostate cancer (or any other male-only cancer). The usual test is the so-called PSA (Prostate Specific Antigen) test, which is a blood test.
Men over 50 are advised to consider having a PSA test for prostate cancer. You may “consider” this by having a discussion with your GP, or by reading readily available advice on-line, e.g., this on prostate cancer or this on the PSA test. The need for you to be pro-active in this matter is made explicit in the official guidance, which states,
GPs should not proactively raise the issue with asymptomatic men.
You are not always best advised to have a PSA test, because the rate of false positives and false negatives are fairly high. So if you have no symptoms, no familial history, and are not black, then you may reasonably opt not to have a test – at least until you are older (say over 60).
PSA levels below 4 ng/mL are taken to be “normal”. Higher levels need discussion with your GP. However, for readings between 4 and 10 ng/mL, only 25% of men turn out to have prostate cancer. Above 10 ng/mL the risk is substantially higher, but still far from certain. Unfortunately, whilst readings below 4 ng/mL are reassuring, they are no guarantee that you are cancer-free, false negatives also occur.
If you do want a test, perhaps for peace of mind if you suffer some of the symptoms, then you are entitled to a test under the NHS Prostate Cancer Risk Management Programme. Some GPs, or their practice nurses, may claim that they do not do PSA tests on request. If you are over 50 you may tell them politely that you are entitled to one (they are probably trying to save money).
You should not ejaculate for 48 hours prior to a PSA test, nor have heavy exercise in that period. This is worth noting because, in my experience, GPs surgeries don’t actually tell you this.
The appropriate action if a PSA result is above 4 ng/mL requires discussion with your GP who will take various other factors into account. A digital-rectal examination is common (and not as eye watering as it sounds). If the GP considers the risk to be significant, the next step has (to date) been biopsy.
2. Prostate Biopsy
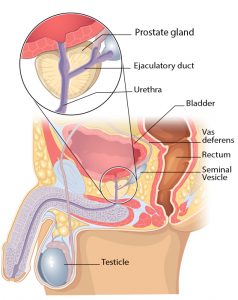
Prostate biopsy involves inserting a needle into the prostate through the wall of the colon. An ultrasound probe inserted in the rectum is used to guide the needle into the correct organ. Yes, it can be painful and carries the risk of bleeding and infection. About a dozen tissue samples are taken. The likelihood of a false positive from a biopsy is very low. However, false negatives are still fairly common, e.g., if, by bad luck, none of the dozen samples happen to hit the tumour.
Around 100,000 men undergo prostate biopsy per year, but rather more than half have a negative result (rightly or wrongly).
3. Enhanced MRI Scans
A particular type of MRI scan, known as a mpMRI (multi-parametric MRI scan) has been shown very recently to be twice as effective as biopsies at spotting prostate cancer. A series of tests on 576 men with raised PSA counts was reported in The Lancet in February 2017. The efficacy of mpMRI was compared with standard biopsy and also with a gold-standard biopsy which took an unusually large number of samples (50 to 60). 40% of the men had clinically significant cancer and mpMRI spotted 93% of these cases compared with only 48% spotted by standard biopsy.
If all 100,000 men annually who are currently given biopsies were given an mpMRI scan first, about a quarter would not need to proceed to biopsy. Moreover, a positive diagnosis from mpMRI assists a subsequent biopsy in correctly locating the tumour which would lead to 37,000 aggressive cancers being picked up, compared to the current 19,000. You don’t have to be a doctor to understand the significance of that. Dr Hasim Ahmed of UCL who led the first mpMRI trials was quoted in The Times (20/1/17) as saying that routine use of mpMRI would likely save the order of thousands of men’s deaths per year.
Angela Culhane, chief executive for Prostate Cancer UK, praised the findings as a ‘huge leap forward’ for the ‘notoriously imperfect’ diagnostic processes currently used. “The results from the (trial) make it clear that giving men with raised PSA an mpMRI scan before a biopsy can help increase the number of aggressive cancers detected whilst reducing the number of unnecessary biopsies for men.This is the biggest leap forward in prostate cancer diagnosis in decades with the potential to save many lives.”
For men to benefit from this new diagnostic technique, hospitals need to have the equipment, and the trained radiology staff to drive it. This is something which men’s activists need to get behind. It’s about time we did more positive campaigning on matters such as this.
4. Targeted drug treatment via blood test
The drugs abiraterone and enzalutamide are given to men whose cancer is no longer responding to traditional hormone therapy and has started to spread. But in some men these drugs do not work well and the disease rapidly returns. Currently, there is no approved test to help doctors choose whether these are the best treatments for an individual.
A cheap blood test has now been developed which can be used to pick out which men are likely to respond to abiraterone and enzalutamide, and which men might need alternative treatments. The test is based on the finding that men with multiple copies of a particular gene do not respond to these particular drugs.
Abiraterone and enzalutamide can be excellent treatments for advanced prostate cancer and some men can take these drugs for years without seeing a return of their cancer. But not so for everyone. Dr Iain Frame, director of research at Prostate Cancer UK, said the test could be a significant step towards moving away from a “one-size-fits-all” approach to treatment.
5. Robotic surgery
Surgical removal of prostate tumours is fraught with post-operative side effects, including erectile dysfunction and incontinence. However, for some years now – at least in better equipped hospitals – the use of computer enhanced robots to assist the surgeon has reduced complications significantly. It’s a type of keyhole surgery. The robot allows the surgeon to make highly precise movements inside the incision. This means that the malignant tissue can be removed with an efficiency and ease unheard of prior to the era of robotic surgery. This greater precision reduces the likelihood of relapse due to missed cancerous tissue. It also helps avoid damaging healthy prostate tissue, which improves clinical results.
6. Transformative laser/bacteria treatment
Even robotic surgery continues to carry the risk of side effects – sufficient to deter a substantial number of men from this option. However, a completely novel type of treatment is now emerging from trials which dramatically reduces the likelihood of any long term side effects, and also has a high success rate of complete remission.
The new treatment is snappily named “padeliporfin vascular-targeted photodynamic therapy”. It uses a drug, made from bacteria that live in the almost total darkness of the seafloor and which become toxic only when exposed to light. The drug is therefore administered in near-darkness.
Ten fibre optic lasers are inserted through the perineum – the gap between the anus and the scrotum – and into the cancerous prostate gland. When the red laser is switched on, it activates the drug to kill the cancer and leaves the healthy prostate behind.
The video of Professor Mark Emberton in this report is worth a listen for further clarification.
Trials on 413 men – published in The Lancet Oncology – showed about half of them had no remaining trace of cancer.
However, the new treatment is not yet available for patients as it is still being assessed. This may be another area where men’s activists could usefully get involved – if availability is prevented on grounds of cost.
Men need an external enemy to promote their in group preference. Look at European history – all against all for hundreds of years until an external threat threatened all, then their was compromise and cooperation. Who could we find who is inimical to all men? Who explicitly and implicitly is against all of us? Tricky – does anyone have a body of evidence demonstrating a political movement that has this amongst their goals? Dare I speak the name of whinem and feminism?
Pingback: Men’s Access to Healthcare | The Illustrated Empathy Gap
Thank you for posting this, Mr Collins.
If men’s advocates are reluctant to put *any* pressure on Cancer Research UK over their “Men & Boys are *BANNED* from participating in hundreds of our events around the country” policy… I think, unfortunately, that it’s very unlikely the MRM/MHRM is even slightly close to creating, or getting behind, campaigns to encourage the usage of new diagnostic techniques, equipment and staff training.
I presume you allude to the Race for Life – the fun runs in aid of breast cancer? These are indeed for women only. They can afford to be – they get many thousands (of women) turning up. They are very successful at raising funds. I have taken part in several similar fun runs for prostate cancer. A friend of mine was instrumental in organising and promoting them. He spared no efforts, including appearances on local radio, giving talks at large offices, and distributing 10,000 leaflets. The results were disappointing, year after year, with only 300 or so turning up, despite support from local radio and TV personalities, etc. Moreover, half of those who ran were women. Men are often criticised for not looking after themselves properly, but the bigger issue is that men do not look after other men at all. So – all that is a long winded way of agreeing with you. The essence of our problems, across the board, is the lack of male in-group preference.