Just a quick snip
This post is the first of a series which will address the claim that circumcision is beneficial in reducing the likelihood of certain diseases. This first part introduces my motivation for revisiting this issue, namely a recent publication by Brian Morris and co-authors. After making some general observations about this journal paper, and setting it in the context of world opinion, I present a specific critique of the claims regarding the impact of circumcision (male genital mutilation, MGM) on urinary tract infections. Part 2 will critique the claims for other diseases. Part 3 will examine the quantifiable risks or disbenefits of circumcision, and hence the overall position on risk-benefit. In addition, Part 3 will present my rebuttals of some appallingly biased counter-arguments to intactivism.
These posts refer to circumcisions carried out by medical practitioners in clean surgical conditions. Some data on traditional Jewish brit milah is included, but this is not the focus of interest. Most importantly, ritual circumcisions of the type which are common in many African countries are not addressed (other than in Part 3 in the context of the cultural context of male circumcision). These latter practices are so brutal, and result so frequently in maimings or death, that any question of the benefit outweighing the risk does not arise at all. (See the links here, for example. Dr Dingeman Rijken’s site includes photographs showing just what “maiming” means. You will need a strong stomach). For companion reading I recommend articles on ExInjuria (and here), especially as regards legal aspects, though that is not my present focus.
**************************
Contents
- Morris et al 2017 – Overview
- Morris et al 2017 – Details
- Morris et al Versus Authoritative Medical Bodies’ Opinion
- Urinary Tract Infections (UTIs)
- 4.1 The Obvious Sexism of the Argument
- 4.2 Does MGM Reduce UTI Incidence?
- 4.3 Summary of the Position re: UTIs
1. Morris et al 2017 – Overview
I have posted on MGM previously. My attention was drawn again to this issue by an Australian news article, World Journal of Clinical Pediatrics study finds evidence in favour of male infant circumcision. The title gives you the gist of it. My attention was grabbed by the following extraordinary claim: “uncircumcised males face an 80 per cent risk of developing a foreskin-related condition requiring medical attention“. It would seem that I’ve been rather lucky. Elsewhere the weaker, but still surprising claim is that “over their lifetime more than one in two uncircumcised males will suffer an adverse medical condition caused by their foreskin“. I shall make a point of asking uncircumcised friends of their own experience. It will not require many to test claims so extraordinary as 80% or 50%.
The study from which these claims are taken is “Early infant male circumcision: Systematic review, risk-benefit analysis, and progress in policy” by Brian Morris and eight co-authors, published in February 2017.
The authors are members of the Circumcision Academy of Australia. Brian Morris is a founding member of the Circumcision Foundation of Australia (which changed its name to the Circumcision Academy of Australia in 2014). I suggest that one does not found a circumcision academy if one is neutral on the matter.
In a letter to the editor of the Canadian Journal of Urology from Joan Robinson and others, it is revealed that the two Canadian co-authors of the paper operate circumcision clinics, which represents an obvious conflict of interest. (This does not preclude other co-authors having similar conflicts of interests, I just don’t know).
One of the more distressing phenomena of our times is that of ‘advocacy research’. At one time, the point of publications was the pursuit of truth. Whilst there has never been a shortage of difference of opinion, the common goal used to be the truth. The intellectual corruption of the postmodern age tells us there is no such thing as truth. This provides spurious legitimacy to those who wish to make science a vector for their propaganda. There is now so much ‘advocacy research’ that it cannot be rooted out: the bind weed is throttling the entire garden. I worry that the scientific process itself is under threat, for publications are the medium through which the informal consensus is established which is the key element in the scientific process. Is the literature becoming too heavily polluted to support meaningful consensus arising anymore? The death of science would be a decisive victory for the nihilistic so-called progressives. This is my nightmare.
I have often wondered why it is that some men seem so very keen to chop off boys’ foreskins. I confess I harbour a suspicion that their motivation might be that, not having a foreskin themselves, they’re damned if other men are going to have one either. What I had not imagined previously was that there might be some perverse sexual gratification involved. I am all too innocent about such things, but apparently there are such people as circumsexuals who enjoy circumfetishism. Some claims have been made that Brian Morris is associated with such groups, though I make no allegation.
However, Dr Morris is certainly an unusually energetic pro-circumcision activist. When interviewed for the above news article he said circumcision was a desirable public health intervention, and moreover would save money. “The enormous benefit but low risk makes early infant circumcision akin to childhood vaccination,” he claimed.
2. Morris et al 2017 – Details
On the face of it, Morris et al (2017) is a properly structured meta-analysis, taking its evidence from a large number of published works. Whilst some of these involve Morris or his co-authors, most do not. So the claims of the paper cannot just be dismissed out-of-hand. Rather it is necessary to consider the arguments and evidence presented on their merits. Unfortunately this takes considerable labour.
The heart of the paper is Table 1, reproduced as Figure 1 below.
Figure 1 (Table 1 from Morris et al 2017) click to enlarge
This Table shows the origin of the claim that uncircumcised males face an ~80% risk of being affected by a disease as a result of having a foreskin. This figure is obtained by summing the ‘percent affected’ in Figure 1 for each listed disease. (Anyone used to dealing with probabilities will be wary of such a naive addition since, with a slightly longer list, a total in excess of 100% could easily result. I suggest that the implied probabilities are best interpreted as expectation values of the number of incidents of disease per man, which can exceed 1). The largest single contributor to this total ‘percent affected’ is urinary tract infections (UTIs) at 27% over life – hence my focus on UTIs in this first post. These ‘percentages affected’ are the claimed benefit of circumcision because, the paper claims, these diseases would not have occurred if the foreskin had been removed.
The claim is being made that, over life, uncircumcised men have an 80% probability of suffering a condition requiring medical attention which they would not have had if circumcised. Elimination of this 80% probability is therefore the claimed benefit of circumcision. (In more coherent language, I suggest this should be expressed as “circumcision reduces the expectation value of the number of incidents of disease by 0.8 per man on average”).
The other side of the coin is the risk of circumcision. Morris et al also make claims on the frequency of risks and disbenefits of circumcision. Their position on disbenefits is simple – there aren’t any, they claim. These issues will be addressed in Part 3. For now we note a major methodological flaw in Morris et al (2017), namely that no account is taken of severity – either of the obviated diseases or of the attendant risks of circumcision. They claim a benefit to risk ratio of ~200 defined as the frequency of offset disease divided by the frequency of circumcision complications.
But failing to address relative severity is clearly bonkers, both for the benefit and the risk side of the equation. The benefit (if there were one) of avoiding cancer is obviously of greater weight than that of avoiding a minor dose of UTI. As regards risk, bleeding to death is obviously of greater weight than a temporary inflammation.
The other methodological problem with Morris et al is that no account is taken of treatability. Most of the 0.8 diseases per man claimed to be avoided by circumcision are easily treated, or obviated, by other means – as we shall see in the details which follow. In contrast, any disbenefits of circumcision, e.g., in terms of loss of sexual function, are largely untreatable and permanent (though I believe that foreskin restoration is increasingly successful, so this may be a slight overstatement).
3. Morris et al Versus Authoritative Medical Bodies’ Opinion
Morris et al (2017) represented the view of the American Academy of Pediatrics (AAP) in a light favourable to circumcision, referring to the AAP’s “formulation and release of a new affirmative early infant MC policy statement in 2012“. The actual view of the AAP is as follows,
“The American Academy of Pediatrics found the health benefits of newborn male circumcision outweigh the risks, but the benefits are not great enough to recommend universal newborn circumcision“.
The AAP’s stance that circumcision carries a net benefit over its risks has been echoed by the US Centre for Disease Control (CDC), and these bodies have come under fire for this interpretation, for example from Brian Earp and Circumcision Information Australia. The CDC have, for example, advised that MGM is beneficial in reducing the risk of various diseases. The CDC write in their advice,
“Parents and guardians should be informed about the medical benefits and risks of neonatal, pediatric, or adolescent medically performed male circumcision. During infancy, circumcised infants are less likely than uncircumcised infants to experience urinary tract infections (UTIs), although UTIs are uncommon during infancy.”
They go on to list benefits to other diseases.
Morris et al (2017) represent the CDC position as being more supportive of their own hard-line pro-circumcision stance than is actually the case. But, like the AAP, the CDC stops short of actually recommending circumcision, the advice being rather bland…
“Health benefits and risks of elective neonatal, pediatric, or adolescent male circumcision should be considered in consultation with medical providers. In the case of discussion about neonatal circumcision, ideally such discussion should occur prior to the birth of the child. Ultimately, whether to circumcise a male neonate or child is a decision made by parents or guardians on behalf of their newborn son or dependent child.”
Morris et al (2017) include this statement,
“Australia is the only non-United States country in which an evidence based policy statement has been produced (by the Circumcision Academy of Australia; CAA). The authors of the policy included fellows of the Royal Australasian College of Physicians (RACP), as well as fellows of other Colleges and medical bodies. The conclusions reached were similar to those of the AAP and CDC.”
Well, the Circumcision Academy of Australia is hardly an unbiased body, having been co-founded by Morris himself. This statement rather upset the RACP – at least I think I can conclude so, reading between the lines. The Australian news article referred to above did not originally include a quote from the RACP, but it was later amended to do so. The RACP disagreed with Professor Morris’ comments, saying the level of protection offered by circumcision did not warrant a change of policy, being quoted thus,
“The RACP believes that the frequency of diseases modifiable by circumcision, the level of protection offered by circumcision and the complication rates of circumcision do not warrant routine infant circumcision for healthy male infants in Australia and New Zealand.”
This is not the first time that Morris and friends have been taken to task by authoritative medical bodies for misrepresenting their position in published work. For example, a 2016 paper “Canadian Paediatrics Society (CPS) position statement on newborn circumcision: a risk-benefit analysis revisited” so upset the CPS that three members of the CPS wrote a detailed rebuttal in a letter to the editor of the Canadian Journal of Urology. Noting that neonatal circumcision is an operation with lifelong consequences performed without patient consent, and further noting deaths from surgical circumcisions in Canada as elsewhere, the CPS authors conclude that the existing evidence fails to provide a case for the CPS to recommend routine circumcision.
Morris et al’s claim that “Australia is the only non-United States country in which an evidence based policy statement has been produced” is rather odd given the statements made by authoritative medical establishments in New Zealand, Canada, Finland, the Netherlands, and, of course, Great Britain – to name just a few – as summarised here. They bear repeating,
- Canadian Paediatric Society (1996): “The overall evidence of the benefits and harms of circumcision is so evenly balanced that it does not support recommending circumcision as a routine procedure for newborns.” This advice was reviewed in 2015, their updated position being, “Recent evidence suggesting the potential benefit of circumcision in preventing urinary tract infection and some sexually transmitted infections, including HIV, has prompted the Canadian Paediatric Society to review the current medical literature in this regard. While there may be a benefit for some boys in high-risk populations and circumstances where the procedure could be considered for disease reduction or treatment, the Canadian Paediatric Society does not recommend the routine circumcision of every newborn male.“
- The Central Union for Child Welfare, Finland (2003): “Circumcision of boys that violates the personal integrity of the boys is not acceptable unless it is done for medical reasons to treat an illness. The basis for the measures of a society must be an unconditional respect for the bodily integrity of an under-aged person. Circumcision intervenes in the sexual integrity of a male child causing a permanent change in organs and has consequences pertaining to both health and quality of life. The circumcision of girls is rightly considered as inhuman mutilation of the genitals and is punished abuse. Also boys must be guaranteed a similar protection by law. According to the opinion of the Central Union for Child Welfare in Finland nobody has the right, on behalf of the child, to consent to operation, violating the bodily integrity of the child, if it is not done to treat an illness.“ In one legal case in Finland in 2006, a circumcision of a four year old boy was ruled illegal. The court noted that “not even a long religious tradition justifies protecting the bodily inviolability of boys to a lesser degree than that of girls“. It is not clear that this makes MGM illegal generally in Finland.
- The Royal Dutch Medical Society (2010): “There is no convincing evidence that circumcision is useful or necessary in terms of prevention or hygiene. Partly in the light of the complications which can arise during or after circumcision, circumcision is not justifiable except on medical/therapeutic grounds. Non-therapeutic circumcision of male minors is contrary to the rule that minors may only be exposed to medical treatments if illness or abnormalities are present, or if it can be convincingly demonstrated that the medical intervention is in the interest of the child, as in the case of vaccinations. Non-therapeutic circumcision of male minors conflicts with the child’s right to autonomy and physical integrity. There are good reasons for a legal prohibition of non-therapeutic circumcision of male minors, as exists for female genital mutilation.”
- British Medical Association (advice dated 2006 but still linked by the BMA site in 2016): “In the past, circumcision of boys has been considered to be either medically or socially beneficial or, at least, neutral. The general perception has been that no significant harm was caused to the child and therefore with appropriate consent it could be carried out. The medical benefits previously claimed, however, have not been convincingly proven, and it is now widely accepted, including by the BMA, that this surgical procedure has medical and psychological risks. It is essential that doctors perform male circumcision only where this is demonstrably in the best interests of the child.”
The bottom line is this: as far as I am aware, no country outside Africa has promoted the routine circumcision of males.
Despite not advising circumcision as a general preventative procedure, medical authorities in many countries do entertain the idea that circumcision can be medically beneficial. I now turn to look at this in detail, starting in this post with urinary tract infections. The remaining diseases will be addressed in a subsequent post.
4. Urinary Tract Infections (UTIs)
4.1 The Obvious Sexism of the Argument
In the first few months of life, UTIs are more common in boy babies than girls. However, after a few months UTIs become substantially more common in females. This continues throughout life, with the incidence of UTIs in females being three or four times that in males, averaged over life. For boys and young men, UTIs are of particularly low frequency. UK NHS data indicates that,
- 3% of girls and 1% of boys will have an upper UTI by the age of 7;
- 10% of girls and 3% of boys will have a UTI by the age of 16.
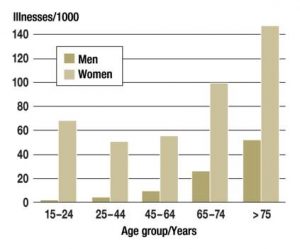
The incidence of UTIs, contrasting the two sexes, is illustrated by Figure 2 taken from this paper in Deutsches Arzteblatt and based on Dutch data. Note that the Netherlands has a very low prevalence of circumcision. The very low occurrence of UTIs in males under 45 years old raises the obvious question: against what threat to males is circumcision supposed to be protecting? There is relatively little risk to males, as opposed to females, below the age of 45.
Figure 2: Frequency of UTIs in the Two Sexes by Age click to enlarge
Figure 2 immediately raises a problem for proponents of prophylactic circumcision: if the foreskin ’causes’ UTI, why do men under ~45 years old get away with it?
UTIs are successfully treated using antibiotics (for both males and females).
I have no idea whether some form of genital mutilation of girls might protect against UTIs. Suppose there were such a procedure: would anyone be in favour of FGM as a preventative of UTIs in females? I don’t think so. Certainly I would not. We have a perfectly adequate means of treating UTIs already. But given that the prevalence of UTIs in females is far larger than in males, how can this be consistent with condoning male circumcision on the basis of UTI prevention? Logically it cannot. And yet some people do condone it. This is only possible because of the empathy gap. Assuming effective UTI prevention were to be realised, the mutilation of males is perceived as acceptable but that of females is not, despite far less benefit accruing to males.
This observation alone exposes the fraudulence of attempting to justify MGM using UTIs – or, indeed, any medical condition which is treatable in another manner. Such arguments are not reasons but post-hoc rationalisations. The unwillingness to apply parallel arguments to females, despite potentially greater benefits, illustrates the contrast between gynocentrism and male disposability.
This conclusion applies irrespective of whether circumcision does or does not significantly reduce the incidence of UTIs. Nevertheless, the evidence in this respect will be reviewed.
4.2 Does MGM Reduce UTI Incidence?
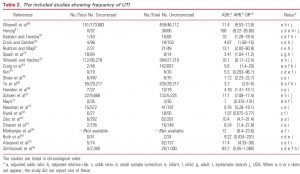
The main reference used by Morris et al (2017) to support their claims about UTIs is one of Brian Morris’s own papers, “Circumcision and Lifetime Risk of Urinary Tract Infection: A Systematic Review and Meta-Analysis“, by Morris and Wiswell (2013). Their case is summarised in their Table 2, reproduced below as Figure 3. This lists 22 references from which relevant data have been extracted in a meta-analysis. It is worth first making some general points about the diagnosis of UTIs.
Figure 3: From Morris & Wiswell (2013) click to enlarge
Adults, or older children, will report symptoms. This may or may not be followed by other diagnostic tests. However, in the case of infants, biochemical diagnostic testing is virtually obligatory since infants cannot communicate their symptoms (though fever will be evident in many). There are two classes of diagnostic test in common use: urine testing with dip sticks and urinalysis. The latter involves growing bacteria cultures from a urine sample.
Dip sticks are not desperately reliable. False positives occur on average ~20% of the time, whilst false negatives are alarmingly frequent, about 43% of the time (see here). Bacterial cultures are therefore the more reliable method.
However, both methods are subject to error depending upon how the urine sample is collected. A catheterised patient is not a suitable subject since the presence of the catheter itself will promote bacterial contamination. Also it is possible for a urine sample to pick up contamination outside the body, giving a false indication. For this reason samples are specified as ‘midstream’ – but even then contamination is possible. In fact, in infants and young boys where the foreskin is not retractable, it will generally be the case that the urine stream plays over the tip of the foreskin prior to collection, making such a sample useless as an indication of internal infection. There is an obvious danger that urine cultures in such cases are merely an indirect means of foreskin detection – positive cultures not necessarily being indicative of internal infection.
Consequently the only data which can be assumed reliable in the case of infants or very young boys will be those where urine samples have been obtained by suprapubic bladder aspiration. This is a procedure in which a needle is inserted into the bladder through the abdomen wall under local anaesthetic (a video of the procedure can be found here).
Table 3 of Morris & Wiswell (2013) indicates the definition of UTI deployed for each of the contributing 22 source references. None involve only suprapubic bladder aspiration. This technique was used in 8 studies, but in all of these cases data was also obtained from other procedures (in 5 cases involving catheters) so it is not possible to judge the reliability of the resulting data. Two further studies used catheters, whilst the remaining 12 studies used unspecified techniques. In short, none of the data used by Morris & Wiswell (2013) is completely sound from the perspective of potential contamination.
Another significant feature of the 22 sources used by Morris & Wiswell (2013) is that there is a dearth of data from adult men. Of the 22 studies, 15 involved only infants, mostly under 1 year and a few up to 4 years old. A further 6 studies involved boys, not exceeding 18 years but mostly younger. Only one study was of adult men. It is noteworthy that this latter study (Spach et al), with very sparse data, produced one of the least effects of circumcision (see Figure 3). Referring to Figure 2 and §4.1, and indeed to the data of Morris et al (2017) in Figure 1, the incidence of UTIs in very young boys and infants is only roughly 1%, whilst in boys up to 18 years it is roughly 3%. And yet Morris et al (2017) claim that the reduction in UTI rate from infants and boys is applicable to adult men, whose base rate of UTI is far higher (28% according to Figure 1). The latter completely dominates the predicted effect, but there is very little data on the effect of circumcision for adult men. This is odd because it is far easier to obtain a clean urine sample from adults.
There is yet another major problem with UTI evidence based on urinalysis. Even when a correct urinalysis is conducted on a clean sample, bacteria in urine does not necessarily imply sickness. In fact, asymptomatic bacteriuria (ABU) is very common. The frequency varies among different populations, depending on factors such as age, sex, and underlying disorders. This source gives the frequency of ABU in different populations is as follows:
- Preschool girls, <2%
- Pregnant women, 2-9.5%
- Women aged 65-80 years, 18-43%
- Men aged 65-80 years, 1.5-15.3%
- Women older than 80 years, 18-43%
- Men older than 80 years, 5.4-21%
A UK NHS source indicates that the prevalence of bacteriuria increases over the age of 65 and does not equate to a diagnosis of a UTI. Alone it is not usually an indication for treatment. In the population aged over 65, bacteriuria may be so high that urine culture ceases to be a diagnostic test. NICE estimates that 10% of men and 20% of women over the age of 65 years have asymptomatic bacteriuria.
Finally, I note that of the 22 sources used by Morris & Wiswell (2013), 19 relate to countries which are culturally dominated by circumcision practice (USA, Iran, Turkey and South Korea). Of the remaining 4 sources, 3 have a high circumcision rate of ~30% (Canada and Australia). It is reasonable to question whether local cultural practice has prejudiced the scientific neutrality of the researchers. I have not examined whether the authors of the studies, or their funding bodies, have conflicting vested interests.
Brit Milah
It was not part of my intention to attempt to distinguish between circumcisions carried out by doctors as a surgical process and those carried out by traditional mohels in brit milah. However I stumbled across a couple of papers, both fairly recent, which bear a mention.
Firstly, an article by Prais, Shoov-Furman and Amir of the Department of Pediatrics, Schneider Children’s Medical Center of Israel: Arch Dis Child. 94(3):191-4 (2009), “Is ritual circumcision a risk factor for neonatal urinary tract infections“. They conclude,
“Although circumcision is commonly believed to protect against urinary tract infection (UTI), it is not unusual in neonates in Israel, where almost all male infants are circumcised….we found that UTI occurred in six of the 24 infants circumcised by a physician (25%), and in 42 of the 87 infants (48%) circumcised by a religious authority….UTI seems to occur more frequently after traditional circumcision than after physician-performed circumcision.” (The apparently high absolute frequency of UTI here is due to deliberate selection of infants with UTI, so is not significant. The significant finding is the relative frequency of UTI after surgical versus traditional circumcision).
The second paper is by Toket and five co-authors of the Department of Pediatrics, Shaare Zedek Medical Center, affiliated with Hadassah-Hebrew University Medical School, Jerusalem, Israel: Isr Med Assoc J. 12(5):262-5 (2010), “A costly covenant: ritual circumcision and urinary tract infection“. They conclude,
“All available medical records of neonates presenting to the pediatric emergency room for evaluation of fever over a 10 year period were reviewed….Among neonates older than 8 days of age, 60 (24.7%) of the 243 febrile Jewish males had a UTI, as compared to 12 (8.4%) of 143 females (P < 0.0001). In 39 of 54 male neonates (72%) for whom circumcision was performed ritually on the eighth day of life, UTI occurred within 9 days of the circumcision. For females, there was no such clustering of UTI cases in the second week of life, nor during any other time period….Febrile male neonates who have undergone ritual circumcision have a high prevalence of UTI.”
Speculation
One of the most striking features about the epidemiology of UTIs is the relative prevalence of UTIs in the two sexes. It is consistently found that male babies are subject to significantly more UTIs in the first couple of months of life, whilst females are overwhelmingly the dominant sufferers from UTI by 1 year, and this remains true throughout life thereafter (Figure 2). One might hypothesise that these two conflicting observations could be causally related. Does the greater exposure of very young male babies to uterine bacteria result in their greater resistance to UTIs thereafter?
The idea is not obviously crazy. We are all used to the idea that modern hygienic living accommodation, resulting in low exposure of children to infectious species, might be causing a rise in certain medical conditions in later life, e.g., asthma. Perhaps the foreskin does provide a bacteria-rich environment – leading to initially higher incidence of UTIs in boy babies – but that, paradoxically, this is ultimately beneficial in terms of increased resistance after the first few months. This is pure speculation on my part, though I note there have been papers claiming benefits of the foreskin in reducing UTIs. If true, circumcision would ultimately be disbeneficial to UTI incidence. This hypothesis has not been tested by the existing data, as far as I can tell, because the data is dominated by infants rather than adults.
4.3 Summary of the Position re: UTIs
In short, whilst the studies underlying the claims of Morris et al (2017) ostensibly provide support for a significant effect of MGM on the incidence of UTIs, there is a range of reasons to regard the evidence as unsafe. A fair summary of the position with respect to UTIs has been provided by representatives of the Canadian Pediatric Society, as follows,
“Circumcision prevents urinary tract infections (UTIs) in males of all ages. The literature in this area is difficult to interpret because urines obtained via a midstream or catheter specimen from an uncircumcised male are commonly contaminated by organisms under the foreskin. Evidence for this is that 9% of uncircumcised and 0.5% of circumcised asymptomatic males had bacteriuria later verified by suprapubic urine collection to be falsely positive. If one ignores this limitation, the number needed to circumcise (NNTC) to prevent one UTI was 111 in a 2005 systematic review of boys of all ages. In a more recent systematic review the NNTC was still 73 for studies that included only infants. Prevention of UTI in infancy remains desirable but there is increasing evidence that UTIs do not cause long term renal damage with a normal urinary tract and can generally be treated with outpatient antibiotics.
There is a paucity of data on UTIs in older children or adults. A systematic review claimed a 6.6 fold increase in uncircumcised males 1 – 16 years but it appears that infant data were not able to be excluded from the six studies used to derive this estimate. Evidence for adult males appears to be limited to an observational study of men with urinary symptoms in a Sexually Transmitted Infection (STI) Clinic where 30% of 26 men with UTIs were uncircumcised versus 12% of 50 with other diagnoses. Therefore, there is only very low quality evidence that circumcision prevents UTIs beyond infancy.”
Even if we ignore the problems with the data and take it all at face value, and even if we ignore the potential complications and disbenefits of circumcision, is it sensible to carry out the order of 100 surgical procedures to save having to treat one patient with antibiotics? Obviously not. The former course would be adopted only if there were over-riding cultural, religious or financial reasons favouring circumcision. Medical good sense is clearly against it.
Additional Reading
CIRP.org have a page specific to UTIs, including the history and extensive references – but it has not been updated since 2009.
Though quite old now, in an editorial in American Family Physician Vol.41, pp 817-820 (1990), Martin Altschul gave a good account of The Circumcision Controversy including data which suggests much lower rates of infant UTIs than given by Morris et al.