…and the benefits? Err, none
See Part 1 for the Introduction. Here I continue my critique of the claims by Morris et al (2017) that male circumcision is medically beneficial.
Part 2 addresses all the claimed medical benefits other than urinary tract infections (which were addressed in Part 1). The conditions which are claimed to be ameliorated by male circumcision are summarised in Table 1 of the paper by Morris et al, 2017. They are addressed in turn, as indicated by the Contents list below.
The discussion necessarily dives to some scientific depths. This critique provides an illustration of how journal papers which superficially appear legitimate can actually be promotional material.
People who enjoy a more polemical exposition can look forward to the concluding Part 3 shortly. My earlier, less detailed, observations on MGM generally can be found here.
Throughout I use the terms “circumcision”, MGM (male genital mutilation), and MC (male circumcision) interchangeably.
Contents
- Phimosis
- Balanitis / Candidiasis
- High Risk HPV Infection
- HIV
- Other STDs
- Genital Ulcer Disease (GUD)
- Syphilis
- Trichomonas Vaginalis
- Mycoplasma Genitalium
- Herpes Simplex Virus Type 2 (HSV-2)
- Chancroid
- The Meta-Analysis of Van Howe (2013)
- Penile Cancer
- Prostate Cancer
- Summary
- Appendix: References Casting Doubt on the Benefits of Circumcision for HIV
1. Phimosis
Phimosis is failure of the foreskin to fully retract. In mature males the foreskin should retract so as to expose the entire glans, or ‘head’ of the penis.
It is undeniably true that circumcision will prevent phimosis – since, if you have no foreskin then there can be no problem with its retraction. But this is like arguing that you could avoid having difficulties cleaning your nails by chopping off your fingers. The remark is not entirely flippant. The issue is whether the cure is out of proportion with the seriousness of the problem.
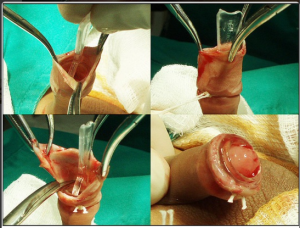
In unmutilated infants the foreskin adheres to the glans. The truly ignorant (who are legion) are unaware that infant circumcision requires that the foreskin is first ripped apart from the glans before it can be cut off. All reputable medical sources are now clear that the foreskin does not, and should not, retract in young boys. Consequently ‘phimosis’ is the natural condition in young boys, not an abnormality. It requires no cure.
However, medical sources still generally under-estimate the age at which full foreskin retraction becomes possible. This UK source states,
“the foreskin cannot normally be retracted completely before the age of 5. In some, full separation may not take place until the age of 10“.
But my personal recollection is that ten year olds generally did not have fully retractable foreskins. This is consistent with advice by cirp.org,
“One may expect 50 percent of ten-year-old boys; 90 percent of 16-year-old boys; and 98-99 percent of 18 year-old males to have full retractable foreskin.”
This Indian source states,
“The foreskin gradually becomes retractable over a variable period of time ranging from birth to 18 years of age or more.”
An old 1968 study by Jacob Øster, summarised here ‘reported on a group of almost two thousand boys aged between 6 and 10 yrs. old. He studied them for a period of 7 to 8 years till they were between 13 and 17 years old. He wrote “phimosis was found in 4% of all observations, but with a diminishing incidence throughout the years, from 8% in 6-7 year-olds, to 1% in 16-17 year-olds.”‘ Øster wrote “Phimosis is seen to be uncommon in schoolboys, and the indications for operation even rarer if the normal development of the prepuce is patiently awaited.” His study showed that phimosis was not necessarily an indication for circumcision.
That the elementary facts about natural foreskin retraction are so uncertain in the literature indicates how neglected male sexual health issues have been. I believe that medical training in the UK makes no mention of the male foreskin whatsoever.
Morris et al claim that 10% of uncircumcised men/boys will develop phimosis.
But there has been enormous confusion between normal juvenile ‘physiological phimosis’ and pathological phimosis. For example, this US source states,
“Current incidence of phimosis is about 1% in 7th grade boys” (hence 12 or 13 years old).
If there are clinical symptoms, such as pain or difficulty urinating, then pathological phimosis might be indicated. But the incidence of normal, developmental phimosis would be expected to exceed the above 1% figure at the age of 12/13.
Robert Van Howe claims that true phimosis occurs in less than 2% of intact males, and in 90% of cases this can be successfully treated with steroid cream. Other treatments short of surgery are also available. As a result, he claims that only 0.07% of boys will require circumcision to rectify phimosis. This is rather different from Morris et al’s claim of 10%, but they not only over-estimate the incidence of phimosis but also refuse to recognise that there is any treatment other than circumcision.
In India, Sukhbir Kaur Shahid notes that,
“The incidence of pathological phimosis is 0.4 per 1000 boys per year or 0.6% of boys are affected by their 15th birthday.”
He also notes the range of anti-inflammatory and hormonal creams available, with efficacy rates in the range 65% to 95% – and if one fails to work, another often will.
Like Van Howe, Shahid also discusses the successes with ‘stretching’ interventions, using “a specially designed patented balloon catheter with local anaesthesia in 512 boys and found it to be 100% useful. The technique was simple, safe, cheap, less painful, and less traumatising then the conventional circumcision. It was found to be more beneficial in younger children with no fibrosis or infection. Combination therapy using stretching and topical steroids has also yielded excellent results.”
Consistent with this, if phimosis has not become pathological, an effective treatment may be to advise conventional masturbation which has the effect of loosening the prepuce and improving its mobility.
In summary,
- Most diagnosed “phimosis” is not pathological phimosis at all, but a natural condition which will disappear with age;
- The incidence of true phimosis is far lower than stated by Morris et al;
- The bulk of cases of true phimosis (~90%) are successfully treated by creams; those few that are not can usually be treated with procedures to loosen the foreskin without requiring its excision;
- The proportion of boys who may ultimately require circumcision to rectify persistent and problematic phimosis is ~0.07%.
I leave the last words to Sukhbir Kaur Shahid,
“Phimosis needs to be differentiated from non-retractile prepuce, which is the rule in young children. Doctors should be taught on distinguishing these two types of phimosis in order to avoid parental anxiety and needless referrals to urologists for circumcisions. Newer nonsurgical modalities such as topical steroids and adhesiolysis are effective, safe, and cheap for phimosis in children. Parents should be made aware of these measures to treat phimosis. If surgery is indeed needed, conservative plastic surgical techniques should be performed rather than the traditional circumcision. This would help the patients, their family, and the healthcare as well as the society at large.”
2. Balanitis / Candidiasis
Balanitis is redness, swelling, soreness or rash around the glans (the head of the penis) or the foreskin. The cause of balanitis is generally poor hygiene.
This NHS source states, amusingly, “other causes of balanitis include…in boys, repeatedly playing with their foreskin“. Well, if this were so, balanitis would be universal. And, in any case, “playing with one’s foreskin” is probably a good way to avoid phimosis. This source observes that “rough handling” may be a cause of balanitis. Indeed.
The incidence of balanitis is almost an irrelevance since effective treatment generally requires merely better hygiene. Cleaning the uncircumcised penis presents no problems. The only people I have ever heard claim otherwise are people without a foreskin. But just because it is very easy to clean does not mean that everyone does so – especially if we are talking about young boys. Soap and water, chaps – and if that doesn’t work, then just warm water (the soap may be the problem).
For persistent cases, antibacterial, or antifungal, or possibly steroidal, creams will be effective almost always.
If re-infection occurs repeatedly after successful treatments, it is likely to be either thrush (candida) or streptococcal bacteria. In both cases the most probable source of infection is the man’s female partner: the vagina tends to harbour these infectious agents. Use of a condom is indicated.
This blog is not supposed to be a source of medical advice (I’m not competent to provide it) but if problems persist the balanitis may be symptomatic of a more serious condition, e.g., diabetes or a more serious STI.
Incidence rates of balanitis are high, around 3% of Western men will experience it. (Some sources quote 11%, but this relates to men seen in urology clinics, and hence is a biased sample).
Morris et al claim that 10% of uncircumcised men will experience balanitis, and that circumcision is 68% effective in preventing it. Oddly, Morris et al list candidiasis as a separate condition, citing a frequency of 10% and that circumcision is 60% effective in preventing it. Both these claims appear exaggerated taken separately, and together especially so.
Wakatsuki suggests that perhaps about half of cases of balanitis are due to thrush (candida), and another 25% are due to streptococcal bacteria. Whilst circumcised men are often said to suffer less frequently from balanitis, they will be equally prone to infection by these agents during sex. Consequently, it seems unlikely that any diminished rate of balanitis amongst circumcised males will be very marked – and some studies suggest that circumcised men actually suffer greater rates of balanitis.
The foreskin protects the glans. It is reasonable to suppose that it might protect from infection. Fleiss et al (1998) argued that the human prepuce does indeed have an immunological function. Its removal would be expected to be disbeneficial as regards infection. The same source pointedly observed that “mass involuntary circumcision has failed to achieve any of the public health benefits its advocates have claimed for it“.
In the case of balanitis, though, the incidence of the condition is relatively unimportant since it is so easily treated. The idea that circumcision could be justified by its effect, if there were any, in reducing the incidence of balanitis is rather preposterous. Nasal surgery is not indicated by the incidence of the common cold.
3. High Risk HPV Infection
There is more than one Human Papilloma Virus (HPV) – at least 170 varieties. Some are asymptomatic, whilst others cause only relatively benign conditions like warts or verrucas. However, at least 18 varieties of HPV cause cancers, mostly of the genitals. These are the high risk varieties. However, one variety, HPV-16, also causes oropharyngeal cancer. The bulk of cervical cancers in women are caused by one or other variety of HPV.
HPV is the commonest of sexually transmitted diseases. Prevalence is extremely high, with some sources claiming that most sexually active men and women will probably acquire genital HPV at some point in their lives. The proportion of women infected with one of the high risk HPVs at any instant has been estimated at ~15%.
Vaccines are available, but are effective only before exposure to the virus. The high risk HPVs are sexually transmitted, so vaccination must be carried out prior to the commencement of sexual activity. For this reason, girls aged 12/13 in the UK are offered vaccination against HPV on the NHS, via school programmes, the uptake being almost 87% as of 2013/14. This has led to falls in the number of pre-cancerous abnormalities of the cervix among vaccinated girls.
Because the vaccine used is effective only for certain varieties of HPV, not all, females also continue to receive cervical smear tests on the NHS as part of a national screening programme.
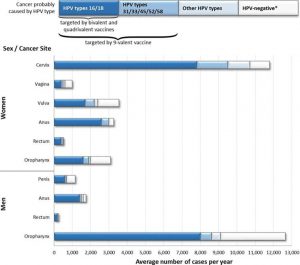
Boys are not vaccinated despite oropharyngeal and other cancers being as strongly associated with HPV as cervical cancer – and despite oropharyngeal cancer being far more common in males. The vaccine used for girls, Gardasil, is effective against HPV-16 which causes oropharyngeal cancers, hence the same vaccine would be efficacious against the main threat to males. Professor Harald zur Hausen, the German virologist who identified HPV as the cause of cervical cancers has said that boys should also be protected by vaccination, but to no effect yet in the UK.
US data from the Centre for Disease Control indicate that the incidence of oropharyngeal cancers in males has now overtaken that of cervical cancers, see Figure 1. In the UK, the incidence of oropharyngeal cancers in males (25 per 100,000 per year) is double the incidence of cervical cancers in females (12 per 100,000 per year).
It has been argued that, “it is only necessary to vaccinate girls because, once vaccination take-up exceeds 80%, ‘herd protection’ ensures that boys are automatically also protected against HPV infection“. One wonders how impressed the feminist lobby would be with that argument if the sexes were reversed.
Figure 1: Incidence of Cancers Caused by HPV in Males and Females (USA)
click to enlarge
And so what about circumcision? Well, there is simply no need to consider Morris et all‘s claims at all, is there? The threat to men is oropharyngeal cancer acquired by oral sex – see Figure 1. Overwhelmingly this is by heterosexual sex, and hence by direct oral contact with female genitalia. The foreskin – indeed the penis – does not come into it (so to speak).
In summary, as regards the HPV cancer risk to men,
- the commonest HPV-cancer is in men;
- in the UK, girls are vaccinated, boys are not;
- in the UK, women have a screening programme, men do not;
- but it’s OK because boys can get bits of penis cut off instead…..eh?
The coup de grace is twits like Brian Morris claiming that chopping off bits of penis can provide protection against HPV whose dominant risk to men is orally acquired oropharyngeal cancer.
But there are no male disadvantages and I’m just a conspiracy nutjob. Right. Got it.
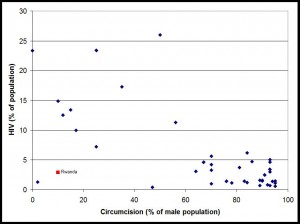
4. HIV
The prevalence of HIV in UK adults is 0.16%. Morris et al cite both 0.2% and 0.1% (presumably relating to Anglophone countries). In respect of the discussion below, note that HIV prevalence in African nations is far, far higher (Figure 2). Even in African countries with in excess of 90% of men circumcised, HIV prevalence on average is ~2.5%, about 15 times higher than in the UK where only 16% of men are circumcised. Not an auspicious starting point for any claims that circumcision is an effective preventative of HIV.
(Aside: Caution must be exercised before concluding that Figure 2 suggests a causal relationship between HIV and circumcision. Differing circumcision percentages reflect differing cultures, e.g., dominant Muslim versus dominant Christian societies, and these will correlate with other cultural differences, e.g., alcohol consumption, women’s free association, etc).
Figure 2: % HIV versus % Circumcision in Africa click to enlarge
Morris et al quote two studies, claiming respectively a 60% and 70% reduction in female-to-male HIV infection rate due to circumcision. The latter paper, claiming the larger benefit, was a meta-analysis by authors from Sichuan University, China,
- Circumcision Status and Risk of HIV Acquisition during Heterosexual Intercourse for Both Males and Females: A Meta-Analysis, Lei et al, PLoS One. 2015; 10(5): e0125436 (May 2015).
This meta-analysis confirms previous work that circumcision affords no benefit as regards transmission of HIV from males to females. As regards female-to-male transmission, 9 studies were quoted which reported a protective effect of circumcision for males. However, most of these studies were cross-sectional or case-controlled studies, as opposed to randomised controlled trials (RCTs).
Pause for a moment to consider the safeguards surrounding bringing a new drug to market. Should a surgical intervention be subject to any less safeguards, especially when the surgery involves irreversible removal of body parts? It is relevant, then, to note that RCTs are a crucial part of the regulatory process whereby a new therapeutic can gain access to the drug market. As a result, clinical trials are large and tightly regulated enterprises that have to comply with ethical requirements while maintaining high epistemic standards. Applying this spirit to the claimed benefits of circumcision to HIV transmission, it is really only the RCT studies which count.
Reasonably, then, Lei et al end up by concentrating upon the three RCTs relating to female-to-male transmission, all of which were conducted in Africa.
The other study cited by Morris et al was,
- Cost-effectiveness of newborn circumcision in reducing lifetime HIV risk among U.S. males. PLoS One 2010; 5:e8723, by Sansom et al (January 2010).
This paper is based entirely on the same three African RCTs, so actually provides no additional independent data.
The three African RCTs upon which Morris et al’s claims ultimately depend are the very same studies upon which the World Health Organisation (WHO) based their recommendation for circumcision as an effective HIV preventative in 2007. Consequently I now concentrate on these three RCT studies, thus addressing both Morris et al and the WHO at the same time. These three RCTs are,
- Auvert B, Taljaard D, Lagarde E, et al. “Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: The ANRS 1265 Trial”. PLoS Med 2005;2:e298. (South Africa)
- Bailey, et al, ” Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial”, The Lancet369 (9562): 643–656, February 2007.
- Gray RH, Kigozi G, Serwadda D, et al. “Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial”. Lancet 2007;369:657-666.
These three studies conclude that circumcision reduces female-to-male HIV transmission rates by 60%, 53% and 51% respectively (though the WHO invariably quotes 60%).
On the strength of these studies, the WHO and the Joint United Nations Programme on HIV/AIDS (UNAIDS) have recommended that male circumcision is an efficacious intervention for HIV prevention and rolled out a programme to circumcise 28 million African men. I find it staggering that the WHO can blithely recommend wholesale mutilation of entire populations. But they are doing so. In the five years to December 2015, 10 million African men had been circumcised under the WHO programmes for AIDS prevention in 14 sub-Saharan African nations. The programme was kick-started with a $50 million grant from the Bill and Melinda Gates Foundation.
I find this predilection of the WHO and its supporters for mutilating huge numbers of poor African men to be a particularly nasty form of neo-colonialism. Daniel J Ncayiyana, editor of the South African Medical Journal has observed that, “it is curious and even worrisome that the campaign to circumcise African men seems to be driven by donor funding and researchers from the North.” He was being diplomatic. He meant, I think, “white men telling black men what to do with their bodies”. He has a point.
Before critiquing the underlying studies, it is worth noting that latex condoms, used consistently and correctly, are 98%-99% effective in preventing HIV transmission. Quite how impressed should we be with a mere 60% reduction in HIV transmission due to circumcision – even assuming we could take this at face value (and we can’t)? Circumcision reduces penile sensitivity and many men find that sex using a condom on a circumcised penis is pointless. If being circumcised were to deter men from using condoms, as it well might, the effect would be an increase in HIV transmission, not a decrease.
The three studies have come in for severe criticism on methodological grounds. The vlogger 5hadowfax has produced an excellent video summarising the fatal shortcomings of the trials upon which the WHO/UNAIDS recommendation is based. These are,
- The fact that safe sex advice, and free condoms, were given to the circumcised men only;
- The studies were stopped early, based on early positive findings (termination bias);
- No account was taken of the fact that circumcised men would be sexually inactive for a couple of months while their wounds healed – so inevitably they had less sex than the control group;
- Parallel studies showed an increase in HIV transmission, but these have been side-lined;
- There is reason to believe that many of the researchers had vested interests in a positive outcome;
- Anomalous results which cast doubt on the veracity of subjects’ self-reporting (as explained here);
- That the studies considered female-to-male HIV transmission only, not male-to-female or male-to-male.
It is worth noting that a follow-up study to the Ugandan trials of Gray et al was carried out, as reported in “The effectiveness of male circumcision for HIV prevention and effects on risk behaviors in a post-trial follow up study in Rakai, Uganda”, Gray et al, AIDS. 2012 Mar 13; 26(5): 609–615 (January 2015). The claim from this study is that similar benefits of circumcision (MC) were observed, and moreover this study confirmed the benefit over a longer period of time. Extracts,
“Following trial closure we offered MC to uncircumcised control arm participants maintained surveillance for up to 4.79 years…..Post-trial HIV incidence was 0.54/100 py in circumcised and 1.71/100 py in uncircumcised control arm men (adjusted effectiveness 67%). There were no significant differences in sociodemographic characteristics and sexual behaviors between controls accepting MC and those remaining uncircumcised.”
A rather obvious problem with this study is that the men who were circumcised were self-selected. The danger, then, is that men accepting circumcision might be those who are more inclined to safe sex practices, e.g., condom use, which would massively skew the findings. Gray et al did attempt to control for this via statistical tests, but I cannot say whether this was necessarily sufficient.
Will the WHO programme of mass circumcisions in Africa be beneficial? As discussed in detail here, in some African nations with initially low rates of circumcision, such as Rwanda, the HIV prevalence is already comparable with that in African nations with 90% or more of men circumcised. Consequently it is hard to see why circumcisions should be beneficial in such nations, but nevertheless the WHO programme is being rolled out. It will be interesting to see, in years to come, whether there has been any benefit from these mass circumcision programmes.
In summary,
- Even if the claim that circumcision reduces HIV transmission by 60% were true, this is hardly adequate to justify wholesale programmes of circumcisions given that condom use is vastly more efficacious (98%-99%).
- This observation is of even greater force in first-world countries with far lower HIV prevalence than African nations.
- The studies implying a 60% reduction are, in any case, so deeply flawed as to have little credibility – and have been widely criticized in the literature (see the Appendix). This has not stopped the WHO and its supporters rolling out a programme of 28 million circumcisions in Africa.
5. Other STDs
Other sexually transmitted diseases which Morris et al claim to be ameliorated by circumcision are genital ulcer disease (GUD), Syphilis, Trichomonas vaginalis, Mycoplasma genitalium, Herpes simplex Type 2 and Chancroid. They claim a decrease in risk of around 50% in most cases (though as low as 15% in some). These are discussed in turn.
As with HIV, the most important point is that condom use provides substantial protection against all these STDs as regards transmission via vaginal intercourse (perhaps 98% – 99% effective assuming invariable and correct usage).
5.1 Genital Ulcer Disease (GUD)
Morris et al cite two sources. One relates to a rather old (1996) study derived from a single clinic in Nairobi (Nasio et al, Int J STD AIDS 1996; 7: 410-414) and indicates roughly a factor of 2 reduction in GUD in circumcised men. The other is Mehta et al “Circumcision status and incident herpes simplex virus type 2 infection, genital ulcer disease, and HIV infection”, AIDS 2012; 26: 1141-1149. Their conclusions include,
“GUD incidence was halved among circumcised men (risk ratio =0.52; 95% CI 0.37–0.73). HSV-2 incidence did not differ by circumcision status (risk ratio =0.94; 95% CI 0.70–1.25).”
This work also suggested a factor of ~2 benefit to GUD conferred by MC.
The null result for Herpes simplex virus Type 2 (HSV-2) is conveniently forgotten by Morris et al when they report on HSV-2 – but they are content to cherry-pick the GUD result which plays to their narrative. This is the difficulty in drawing firm conclusions from a broad literature with conflicting results – and it presents those pursuing an agenda with an ideal opportunity to cherry-pick the bits which support their contentions.
However, in the case of GUD, there probably is a beneficial effect of circumcision. This was the conclusion of Van Howe’s survey of the medical literature on MC and STDs in 1999. Van Howe’s extremely thorough 2013 meta-analysis continues to confirm a beneficial effect of circumcision on GUD. He concludes, “The comparisons of men diagnosed with GUD and GDS (genital discharge syndrome) are consistent with findings that intact men are more prone to GUD and circumcised men are more prone to GDS. Consequently, there is no surprise here“. So, taking GUD and GDS together, there is no benefit.
Van Howe rightly raises the issue of publication bias. He writes,
“A funnel graph, which plots the precision (the inverse of variance) on the y-axis and the natural logarithm of the odds ratio on the x-axis, should have a shape like an inverted funnel with the largest study representing the apex of the inverted funnel. If there is a paucity of studies in the left lower portion of the inverted funnel and a cluster of studies in the right lower portion, that would be suggestive of publication bias…..Paucity in the left lower portion is seen in the funnel graphs for NSU, GUD, syphilis, genital warts and HPV.”
This is worth bearing in mind throughout this review. (Van Howe includes the funnel graphs – see that reference).
5.2 Syphilis
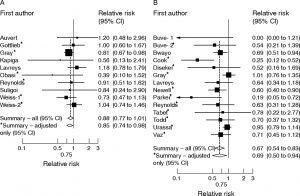
Morris et al cite three sources claiming a reduction in syphilis in circumcised men. That of Weiss et al, “Male circumcision and risk of syphilis, chancroid, and genital herpes: a systematic review and meta-analysis”, Sex Transm Infect. 2006 Apr; 82(2): 101–110 includes the conclusions,
This first systematic review of male circumcision and ulcerative STI strongly indicates that circumcised men are at lower risk of chancroid and syphilis. There is less association with HSV-2…. Most syphilis studies reported a substantially reduced risk among circumcised men (summary RR?=?0.67, 95% confidence interval (CI) 0.54 to 0.83)…. Circumcised men were at lower risk of chancroid in six of seven studies (individual study RRs: 0.12 to 1.11).
However, the detailed results show a less clear picture as regards syphilis. Figure 3 is taken from the paper,
Figure 3: From Weiss et al, 2006 – Relative risk (RR) of circumcision status with (A) HSV-2 and (B) syphilis seropositivity. The square and horizontal line corresponds to the RR and 95% CI for each study. The area of the square reflects the weight of each study. The summary RRs are shown by the diamonds. click to enlarge
Column A in Figure 3 reinforces the lack of benefit for HSV-2.
Column B shows the results for syphilis. Note that, despite the “summary RR” being declared statistically significant, of the 14 studies within the meta-analysis, 11 give results statistically consistent with no effect (i.e., no effect is within the 95% confidence interval). Note that some results fail to overlap.
Using standard statistical calculations, the investigators determined that it was unlikely that the variation of the RR among the studies was due to chance (P = 0.01). In other words, differences in how the studies were designed and conducted led to significant variation in the outcomes. Consequently, the authors declared that there was significant heterogeneity among the studies and warned that the summary RR “should be interpreted cautiously.”
The second source cited by Morris et al was Pintyre et al, “Association between male circumcision and incidence of syphilis in men and women: a prospective study in HIV-1 serodiscordant heterosexual African couples”, Lancet Glob Health. 2014 Nov;2(11):e664-71, appears to support the contention, concluding that “male circumcision was associated with decreased risk of incident syphilis in men and women“. However, a close reading of the more detailed presentation of their findings reveals that a statistically significant reduction in syphilitic infection after circumcision was found only in men who already had HIV. In the subset of men without HIV, the association of circumcision with syphilis infection rates was not statistically significant. Hence, this reference fails to support Morris et al’s claim for it. Moreover, this work was funded by the Bill & Melinda Gates Foundation, amongst others. Given their position on circumcision, via support of the WHO programme, one might question if the authors were under pressure as regards the slant of their conclusions.
The third source cited by Morris et al was Otieno-Nyunya et al, “Epidemiology of syphilis in Kenya: results from a nationally representative serological survey”, Sex Transm Infect. 2011 Oct;87(6):521-5. Ostensibly this indicated a relative risk of contracting syphilis of about 2.2 associated with being uncircumcised. However, this study, like that of Pintyre et al, found a strong positive relationship between HIV infection and syphilis infection. The relative risk of catching syphilis due to being uncircumcised appears not to have controlled for HIV – consequently it is likely that, as with Pintyre et al, above, the apparent benefit would disappear for men without HIV. [As an aside, Otieno-Nyunya et al identify substantially larger benefits in terms of reduced risk of syphilis infection to result from both relative wealth and relative educational attainment. Perhaps the Gates Foundation would be better advised to spend their money on schools and improving economic prospects].
The meta-analysis of Van Howe (2013) concludes, “syphilis showed mixed results with studies of prevalence suggesting intact men were at greater risk and studies of incidence suggesting the opposite”. [NB: “Prevalence” is the proportion of people with the disease at any one time, whereas “incidence” is the proportional rate of new cases of the disease]. Taking all results into account, whilst a beneficial effect of circumcision on syphilis infection cannot be ruled out, any such effect is small as well as uncertain. Van Howe ends with the statement, “one cannot accurately conclude that the risk of syphilis is significantly associated with circumcision status”.
5.3 Trichomonas Vaginalis
Morris et al cite as their source Sobngwi-Tambekou et al, “Male circumcision and Neisseria gonorrhoeae, Chlamydia trachomatis and Trichomonas vaginalis: observations after a randomised controlled trial for HIV prevention”, Sex Transm Infect. 2009 Apr;85(2):116-20, claiming a reduction of 50% in the risk of being infected with Trichomonas vaginalis due to being circumcised. What Morris et al fail to mention is that the data of Sobngwi-Tambekou et al fail to pass the usual test of statistical significance (specifically, p = 0.062, the usual test being p < 0.05). Moreover these authors also note that “the association between T vaginalis and male circumcision remained borderline when controlling for age, ethnic group, number of lifetime partners, marital status, condom use and HIV status (p = 0.069)“. Consequently we can simply rule out Morris et al’s claim as invalid.
5.4 Mycoplasma Genitalium
Morris et al cite as their source Mehta et al, “The effect of medical male circumcision on urogenital Mycoplasma genitalium among men in Kisumu, Kenya”, Sex Transm Dis. 2012 Apr;39(4):276-80. They conclude that “being circumcised nearly halved the odds of Mycoplasma genitalium “. However, once again the association was outside the statistical significance criterion (p = 0.06). In any case it is still controversial whether or not this bacterium is truly a sexually transmitted pathogen. It can cause urethritis, but Mehta et al note that it was actually asymptomatic in 98% of their cases. Rather a non-event.
5.5 Herpes Simplex Virus Type 2 (HSV-2)
With HSV-2 we see most clearly the cherry-picking trick in which Morris et al are indulging. There is no need to review the sources they quote (claiming reductions in HSV-2 infection due to circumcision of up to 50%). There is no need because two of the sources reviewed in the context of other diseases have already presented us with the result that circumcision has no effect on HSV-2 infection. And the fact that Morris et al conveniently ignore this awkward fact is the measure of their reliability.
To recap: column A of Figure 3, from the meta-analysis of Weiss et al, 2006 clearly shows no significant effect of circumcision in reducing HSV-2 rates of infection. Prior to that we noted that Mehta et al (2012) concluded, “HSV-2 incidence did not differ by circumcision status“.
But that is not the final word on the matter. There is also the issue of Orthodox Jewish circumcision practices which are known to have caused HSV-2 infection in the unfortunate infants. For example, TIME magazine, June 7, 2012, ran an article by Alexandra Sifferlin, “How 11 New York City Babies Contracted Herpes Through Circumcision”. It reported that,
“An ultra-Orthodox Jewish circumcision ritual is found to cause neonatal herpes infections in newborns in New York City, prompting health officials to encourage parents to consider the health risks of the practice.”
The Orthodox Jewish circumcision ritual in question is called metzitzah b’peh – or oral suction – in which the mohel puts his mouth directly on the newborn’s circumcised penis and sucks away the blood. There are cases of this practice causing herpes infections of the child quite regularly, the latest I am aware of relates to six infected babies. The two mohels who have been identified as responsible, but not named, have not been punished, or banned from practicing as circumcisers, but are ‘on their honour’ to stop metzitzah b’peh. No doubt others will continue.
5.6 Chancroid
Morris et al cite Weiss et al, Sex Transm Infect. 2006 Apr; 82(2): 101–110 which includes the conclusion, “Circumcised men were at lower risk of chancroid in six of seven studies (individual study RRs: 0.12 to 1.11)“. This claim of Weiss et al has been comprehensively demolished in the excellent meta-analysis of Van Howe (see next section). Van Howe writes,
“The paucity of studies, the reliance on clinical identification in all but one of these studies, and the high degree of between-study heterogeneity make it difficult to comment on the impact of circumcision on this illness, yet the lack of good evidence did not keep the 2012 AAP Task Force from including a discussion of circumcision’s impact on the prevalence of chancroid, which is relatively uncommon in developing nations and extremely rare in developed nations.
The data do not support the claim by Weiss et al. that “circumcised men are at lower risk of chancroid”. There have been no new publications on the impact of circumcision on the prevalence of chancroid since 2006. The difference between the analyses is that Weiss et al. included several studies in their meta-analysis that were not strictly studies of chancroid. As I have noted previously, three of the studies included in their analysis of chancroid did not meet basic inclusion criteria because they lacked a direct comparison between intact and circumcision men for a specific diagnosis of chancroid. In two of the studies, men with genital ulcers were presumed to have chancroid but never tested for it, while the third study tested the men presumed to have chancroid and found that 31.4% had herpes simplex virus type 2 and only 22.9% had a positive culture for Haemophilus ducreyi, the causative agent of chancroid. When these studies are appropriately assigned to an analysis of the prevalence of GUD and excluded from an analysis of the prevalence of chancroid, any imagined association between circumcision status and prevalence of chancroid evaporates.”
5.7 The Meta-Analysis of Van Howe (2013)
Robert Van Howe is the best antidote to Brian Morris. His tour de force meta-analysis of 2013 is impressively thorough and carries conviction: “Sexually Transmitted Infections and Male Circumcision: A Systematic Review and Meta-Analysis”, by Robert S. Van Howe, ISRN Urology, Volume 2013, Article 109846. The Abstract from that paper forms a fitting conclusion to this far briefer review of STDs,
“The claim that circumcision reduces the risk of sexually transmitted infections has been repeated so frequently that many believe it is true. A systematic review and meta-analyses were performed on studies of genital discharge syndrome versus genital ulcerative disease, nonspecific urethritis, gonorrhea, chlamydia, genital ulcerative disease, chancroid, syphilis, herpes simplex virus, human papillomavirus, and contracting a sexually transmitted infection of any type. Chlamydia, gonorrhea, genital herpes, and human papillomavirus are not significantly impacted by circumcision. Syphilis showed mixed results with studies of prevalence suggesting intact men were at greater risk and studies of incidence suggesting the opposite. Intact men appear to be of greater risk for genital ulcerative disease while at lower risk for genital discharge syndrome, nonspecific urethritis, genital warts, and the overall risk of any sexually transmitted infection. In studies of general populations, there is no clear or consistent positive impact of circumcision on the risk of individual sexually transmitted infections. Consequently, the prevention of sexually transmitted infections cannot rationally be interpreted as a benefit of circumcision, and any policy of circumcision for the general population to prevent sexually transmitted infections is not supported by the evidence in the medical literature.”
6. Penile Cancer
In the UK, penile cancer is relatively rare – but not, perhaps, as rare as you might imagine. It is virtually unknown before 40 years of age, but thereafter becomes increasingly common. The incidence rate of new cases is about 2 per 100,000 men in the UK population per year, averaged over all ages – but ten times this for the over-80s. However, that low incidence rate still equates to 630 new cases per year in the UK, resulting in 130 deaths, with 1 in 585 men being diagnosed with the disease at some time during their life – probably when quite old. So, whilst relatively rare for a cancer, penile cancer actually kills more men than the total deaths (of men and women) through intimate partner violence. Penile cancer is substantially more prevalent in the lower socioeconomic classes.
The main source on which Morris et al’s claims rest is the meta-analysis of Larke et al, London School of Hygiene and Tropical Medicine, “Male circumcision and penile cancer: a systematic review and meta-analysis”, Cancer causes & control 22 (8). pp. 1097-110, authors Natasha Larke, Sara Thomas, Isabel dos Santos Silva and Helen Weiss. Their conclusions are as follows,
“There was a strong protective effect of childhood/adolescent circumcision on invasive penile cancer. In two studies, the protective effect of childhood/adolescent circumcision on invasive cancer no longer persisted when analyses were restricted to boys with no history of phimosis. In contrast, there was some evidence that circumcision in adulthood was associated with an increased risk of invasive penile cancer. There was little evidence for an association of penile intra-epithelial neoplasia and in situ penile cancer with circumcision performed at any age.”
In other words, their findings were not generally supportive of a beneficial effect of MC on penile cancer. Only in one sub-set of the data was such an effect found (critiqued below). One wonders why the authors were therefore happy to conclude that,
“Expansion of circumcision services in sub-Saharan Africa as an HIV prevention strategy may additionally reduce penile cancer risk.”
Perhaps the following, found under “Acknowledgements”, provides a clue,
“We are grateful to the World Health Organisation for funding this research”
The key to the statistics lies in this sentence in the paper, which I will decode for you,
“We decided a priori to analyse the effect of circumcision on (1) high-grade PIN and in situ penile cancer and (2) invasive penile cancer separately.”
PIN stands for penile intra-epithelial neoplasia. ‘Epithelial’ essentially means ‘skin’, whilst ‘neoplasia’, or dysplasia, refer to abnormal growth of tissue. The term PIN in this context refers to the initial stages of penile cancer, prior to the cancer spreading elsewhere – after which it would be referred to as “invasive penile carcinoma”. PIN comes in degrees of dysplasia, the later stages also being referred to as “in-situ carcinoma”, i.e., a clearly cancerous tissue but which has not yet spread beyond its initiation site.
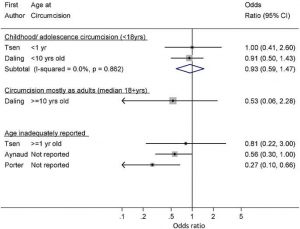
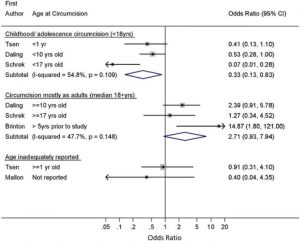
Hence, the above quote from Larke et al means that data referring to PIN or in-situ penile cancer has been analysed separately from data on the later stage of invasive penile carcinoma. Their results are summarised in Figures 4a and 4b for the PIN/in-situ and invasive cases respectively.
Consistent with Larke et al’s stated conclusions, Figure 4a shows no association between circumcision status and PIN/in-situ penile cancer. Six of the seven studies quoted give odds-ratios consistent with equality.
Also consistent with Larke et al’s stated conclusions, Figure 4b shows a disbeneficial association between circumcisions carried out when adult and invasive penile cancer, though of arguable statistical significance. However, ostensibly Figure 4b shows a beneficial association between circumcisions carried out in childhood and invasive penile cancer.
But as regards that last point there is a glaring logical inconsistency with Figure 4a. If circumcision is not associated with the earlier (in-situ) stage of the disease, it cannot possibly be associated with the later (invasive) stage of the cancer. Larke et al appear unconcerned about this logical problem.
What we are probably seeing here is an artefact of dividing the dataset as Larke et al chose to do. Be that as it may, the logical problem identified above is sufficient to fatally compromise the conclusion that MC reduces penile cancer risk.
Figure 4a: Association of MC and PIN or In-Situ Penile Carcinoma – click to enlarge
Figure 4b: Association of MC and Invasive Penile Carcinoma – click to enlarge
7. Prostate Cancer
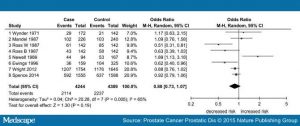
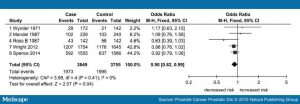
Morris et al quote the meta-analysis results of Pabalan et al “Association of male circumcision with risk of prostate cancer: a meta-analysis”, Prostate Cancer Prostatic Dis. 2015 Dec;18(4):352-7. But, in actual fact, this source finds that – using all the identified studies – the reduced risk associated with MC was not statistically significant (p = 0.19, thus failing the usual requirement for p < 0.05). Whilst the significance improved on the rejection of outliers (to p = 0.04) the odds ratio was then a very marginal 0.9 (i.e., a 10% reduction in risk).
Figures 5a and 5b illustrate the findings, showing the range of odds ratios from the contributing analyses (with and without the outliers respectively). Six of the nine studies in Figure 5a give a result consistent with equity (odds ratio of 1), whilst two more are close to being consistent with equity. Rejecting the outliers (Figure 5b) makes this even clearer.
I have not examined the claims for black people, which appear stronger (41% risk reduction at p = 0.02) – but probably isn’t (see below). However, other than this demographic there appears no strong case in Pabalan et al for a beneficial effect of MC on prostate cancer.
Prostate cancer is a disease of older men; you are very unlikely to get prostate cancer as a young man, and the risk increases sharply after retirement age. Consequently any studies which do not control for age are suspect. Suppose, for sake of argument, that being circumcised reduced your life expectancy. In that case you would see a beneficial effect of circumcision on prostate cancer if you did not control for age – because fewer circumcised men would live to get the disease. Clearly this paradoxical outcome cannot truly be deemed a benefit for the circumcised. Now, whilst circumcision per se is unlikely to reduce your life expectancy, it is possible that in some datasets the prevalence of circumcision is correlated with poorer socioeconomic groups – and these in turn correlated with shorter life expectancy. This would be the case in the UK as a whole, for example. Consequently any studies not controlling for age and socioeconomic group must be suspect.
The shortcomings of other studies claiming a beneficial effect of MC on prostate cancer are expounded here. A far more reliable, and far more pleasurable, means of protecting the health of your prostate is to have regular sex – alone if necessary.
Figure 5a: Overall meta-analysis from Pabalan et al – click to enlarge
Figure 5b: Meta-analysis from Pabalan et al Excluding Outliers – click to enlarge
8. Summary
Some conditions, such as phimosis or balanitis, are either normal, or, if pathological, are easily treated by means less radical than surgery.
That circumcision is not indicated as a preventative for sexually transmitted diseases has been thoroughly argued by Van Howe (2013). The counter-claims by Morris et al have been deconstructed here. Many of those claims result from careful cherry-picking of supportive studies to the exclusion of conflicting studies. In other cases, examining the quoted references reveals that the claims are not statistically significant, often exacerbated by factors which have not been controlled-out. Reporting bias is often evident, and impartiality of some authors may be questioned when their funding bodies are known to have a particular stance on mass circumcision programmes.
I have focussed particularly on the claims made for the efficacy of MC on HIV transmission for this reason, and also in view of its medical seriousness. It is shocking that mass mutilations are being promoted by the WHO based on such suspect evidence. A video by 5hadowfax is recommended as a succinct exposition of the problems with the African studies.
The claims regarding HPV are particularly preposterous because the overwhelming threat to males is through oral infection.
Claims for a beneficial effect of MC on penile and prostate cancers simply do not pass muster on examination of the statistical evidence.
It is rather alarming that a mass delusion on the matter of the medical benefits of circumcision has been perpetrated worldwide, aided and abetted by a weighty epidemiological literature with superficial authority but which appears to me to be contaminated by confirmation bias and vested interests.
Appendix: References Casting Doubt on the Benefits of Circumcision for HIV
- Daniel J Ncayiyana, editor, South African Medical Journal, November 2011, Vol. 101, No. 11, The illusive promise of circumcision to prevent female-to-male HIV infection – not the way to go for South Africa. “Protagonists have touted universal neonatal circumcision (proscribed in South Africa under current law) even though, as cogently argued by Sidler et al.,no credible evidence exists linking circumcision to future protection from HIV in adulthood”.
- In reply to the Co-Director of NOCIRC-SA (National Organisation of Circumcision Information Resource Centres, South Africa) on 23 June 2011, the South African Medical Association wrote the following letter: CIRCUMCISION OF BABIES FOR PROPOSED HIV PREVENTION: The matter was discussed by the members of the Human Rights, Law & Ethics Committee at their previous meeting and they agreed with the content of the letter by NOCIRC SA. The Committee stated that it was unethical and illegal to perform circumcision on infant boys in this instance. In particular, the Committee expressed serious concern that not enough scientifically-based evidence was available to confirm that circumcisions prevented HIV contraction and that the public at large was influenced by incorrect and misrepresented information. The Committee reiterated its view that it did not support circumcision to prevent HIV transmission.
- Robert S. Van Howe and Michelle R. Storms, in How the circumcision solution in Africa will increase HIV infections: “The World Health Organization and UNAIDS have supported circumcision as a preventive for HIV infections in regions with high rates of heterosexually transmitted HIV; however, the circumcision solution has several fundamental flaws that undermine its potential for success. This article explores, in detail, the data on which this recommendation is based, the difficulty in translating results from high risk adults in a research setting to the general public, the impact of risk compensation, and how circumcision compares to existing alternatives. Based on our analysis it is concluded that the circumcision solution is a wasteful distraction that takes resources away from more effective, less expensive, less invasive alternatives. By diverting attention away from more effective interventions, circumcision programs will likely increase the number of HIV infections.“
- Connolly, Catherine; Leickness C. Simbayi, Rebecca Shanmugam, Ayanda Nqeketo (October 2008). “Male circumcision and its relationship to HIV infection in South Africa: Results of a national survey in 2002” (PDF). South African Medical Journal 98 (10): 789–94: “Circumcision had no protective effect in the prevention of HIV transmission. This is a concern, and has implications for the possible adoption of the mass male circumcision strategy both as a public health policy and an HIV prevention strategy.”
- Thomas, A.G.; , L.N. Bakhireva, S.K. Brodine, R.A. Shaffer (11–16 July 2004). “15th International AIDS Conference”. Prevalence of male circumcision and its association with HIV and sexually transmitted infections in a U.S. navy population. Bangkok, Thailand, reported that “male circumcision is not associated with HIV or STI prevention in a U.S. Navy population.”
- Van Howe, Robert; J. Steven Svoboda, Frederick M. Hodges, (November 2005). “HIV infection and circumcision: cutting through the hyperbole”. Journal of the royal society for the promotion of health 125 (6): 259–65: “We contend that the rush to intervene has little to do with preventing HIV infection in Africa and may have more to do with a conscious and/or unconscious impulse to help perpetuate and promote the practice (of circumcision) in North America. There is ample indirect evidence to support this contention. Why are circumcision proponents expending so much time and energy promoting mass circumcision to North Americans when their supposed aim is to prevent HIV in Africa? The circumcision rate is declining in the US, especially on the west coast; the two North American national paediatric organisations have elected not to endorse the practice, and the practice’s legality has been questioned in both the medical and legal literature. ‘Playing the HIV card’ misdirects the fear understandably generated in North Americans by the HIV/AIDS pandemic into a concrete action: the perpetuation of the outdated practice of neonatal circumcision.”
- “Risk behaviors and patterns of HIV seroprevalence in countries with generalized epidemics: Results from the Demographic and Health Surveys”. APHA Scientific Session and Event Listing. 2006: “No consistent relationship between male circumcision and HIV risk was observed in most countries.”
- Way, A.; V. Mishra, R. Hong, K. Johnson (7–12 July 2006). “AIDS 2006 – XVI International AIDS Conference”. Is male circumcision protective of HIV infection?. Toronto, Canada: International Aids Society, “With age, education, wealth status, and a number of sexual and other behavioral risk factors controlled statistically, in only one of the eight countries were circumcised men at a significant advantage. In the other seven countries, the association between circumcision and HIV status was not statistically significant for the male population as a whole.”
- Mills and Siegfried,The Lancet 368 (9543): 1236, concluded that “The circumcision trial is …at risk of serious effect overestimation. We therefore advocate an impartial meta-analysis of individual patients’ data from this and other trials underway before further feasibility studies are done“.
- Brewer, Devon; Potterat, JJ; Roberts Jr, JM; Brody, S (February 2007). “Male and Female Circumcision Associated with Prevalent HIV Infection in Virgins and Adolescents in Kenya, Lesotho, and Tanzania”. Annals of Epidemiology 17 (3): 217–26. “[circumcised] male and female virgins were substantially more likely to be HIV infected than uncircumcised virgins. Among adolescents, regardless of sexual experience, circumcision was just as strongly associated with prevalent HIV infection. However, uncircumcised adults were more likely to be HIV positive than circumcised adults.”
- Gary Dowsett and Murray Couch,Reproductive Health Matters 2007;15(29):33–44, “Male Circumcision and HIV Prevention: Is There Really Enough of the Right Kind of Evidence?” If one believes that male circumcision is efficacious against HIV, the proffered mechanism involves “the susceptibility to HIV in Langerhans cells in the inner foreskin, and a protective keratinisation that occurs after circumcision.” Dowsett and Couch go on to note that Langerhans cells occur in the clitoris and the labia and other parts of female genitalia but no one is talking of mass genital mutilation of females in the name of HIV prevention. Of course not. That would be hateful. Yes, it would.
- Sidler, D.; J. Smith, H. Rode (29 September 2008). “Neonatal circumcision does not reduce HIV/AIDS infection rates” (PDF). South African medical journal 8 (10): 762–766: “Using neonatal non-therapeutic circumcision to combat the HIV crisis in Africa is neither medically nor ethically justifiable. Furthermore, promoting circumcision might worsen the problem by creating a false sense of security and therefore undermining safe sex practices. Education, female economic independence, safe sex practices and consistent condom use are proven effective measures against HIV transmission.”
- Boiley, MC; K Desai1, B Masse, A Gumel (October 2008). “Incremental role of male circumcision on a generalised HIV epidemic through its protective effect against other sexually transmitted infections: from efficacy to effectiveness to population-level impact”. Sexually Transmitted Infections 84 (Supplement 2): ii28–34: “The protection of circumcision against STI contributes little to the overall effect of circumcision on HIV.”